Resources and Tools
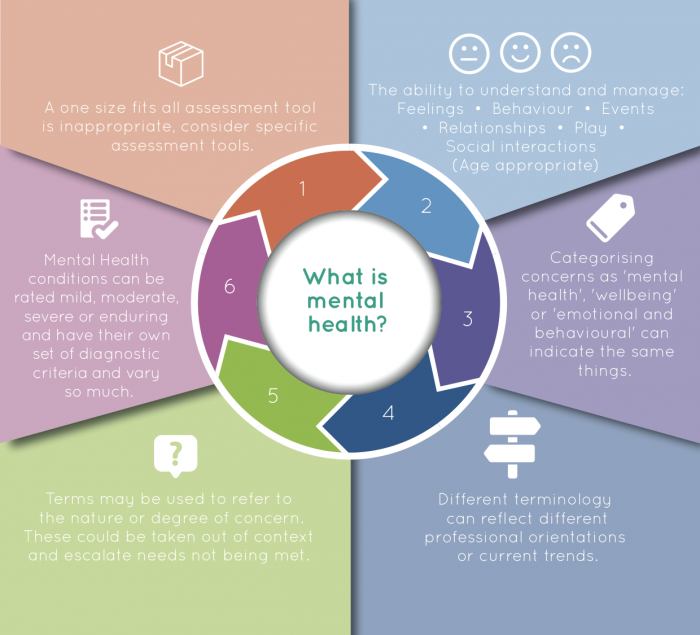
Mental health is the ability to understand and manage feelings, behaviour, events and relationships. Play, social interactions and learning are age appropriate or at the level of an individual’s ability or particular circumstances.
Categorising concerns as ‘Mental Health’, ‘Wellbeing’ or ‘Emotional and Behavioural’, can indicate the same things The use of different terminology sometimes reflects different professional orientations or current trends on the use of language. They are sometimes used to refer to the nature or degree of concern but can occasionally be out of context to a presenting concern which can escalate needs being met at an inappropriate level of service or risk a need being adequately met at all.
‘Mental Health Conditions’ for instance, are often rated as being either ‘Mild, Moderate, Severe or Enduring’. Each category will have its own set of diagnostic criteria for each condition, and these vary so much, that it’s almost impossible to have a ‘one size fits all’ assessment tool to help determine the level of a problem and where an individual’s needs be best metand by who?
‘Supporting Children and young People’s Mental Health and Wellbeing is Everybody’s Business’.
Here are some other Key Messages:
• Feelings are important to children, young people and adults and affect thinking, learning and behaviour.
• Some behaviours can be a child or young person’s solution to coping with a problem.
• Children, young people and adults need to know when and where they can go to seek help.
• Children, young people and adults have a right to be listened to, valued and understood within
respectful relationships.
• Positive mental health is essential to achieving positive outcomes/
• Children, young people whose disability, ethnic background, religious beliefs, culture, life-style, sexual orientation and linguistic needs, may pose an additional barrier in accessing the usual support systems. They require particular consideration when identifying ways to promote and intervene in addressing their mental health and wellbeing concerns.
When considering a pupil’s mental health, there is always a need to question whether there are grounds for considering that this is a ‘child in need’ and/or in ‘danger of significant harm’. Where there arethese grounds for concern then child protection procedures should be followed.
Below is a list of common behaviours that a pupil with mental health difficulties may present with.
- Little pleasure shown at a time when pleasure would be expected
- Being clingy or demanding in school, tearful
- Regression to younger behaviour
- Becoming bossy or over controlling
- Self-harming behaviour
- Becoming withdrawn
- Loss of previously acquired skills
- Substance abuse
- Sudden changes of behaviour, mood or appearance
- Concentration problems
- Relationship difficulties
- Niggley, persistent health complaints with no clear cause
- Problems with losing/gaining weight
- Problems with toilet training or wetting/soiling inappropriate to age or medical issues
- Not very responsive to hurt, loss or pleasure
- Raised or unusual levels of anxiety
- Fighting frequently, temper outbursts
- Deterioration in standards of work
- Insisting on initiating sexual play
- Obsessive ritualistic play
- Destructive of others and own property
- Loss of interest and/or energy
- Disturbed sleep, fatigue, bad dreams
- Feeling worthless, lacking pride
Many of these behaviours could be considered ‘normal reactions’ to transitions, major life eventsand the anniversary of these events. However, some children and young people may need support if:
• these behaviours persist over time (i.e. longer than would normally be expected)
• there are a number of risk factors present (See Alan Carrs’ Risk and Protective Factors Model)
• their behaviours have become a barrier to their learning or the learning of others.
• their behaviours are inhibiting their quality of life
How to Assess and Intervene
Thankfully, we do have local standards and tools to enable assessments i.e. Early Help Assessment. There are also various other assessment tools pertaining to specific concerns available to download or access via the asknormen website, i.e. self-harm pathway (Northampton), GAD 7 (Generalized Anxiety and Depression Scale), HAD (Hospital Anxiety and Depression Scale) and many more to aid a comprehensive assessment of a difficulty or need.
A wealth of resources and tools to assist any interventions with children and young people are available on-line. This section to the asknormen website has been developed for you to readily access some.
It is recommended to consult with the RMC Specialist Primary Mental Health Team or MASH about your concern to seek advice and guidance or to discuss a need to make a referral.
Assessing and providing support with a wellbeing concern which can be met within Early Help/Universal/Targeted/Levels 1 and 2 Services. Whilst this can seem a daunting task at first, it isn’t too difficult and can be achieved by most professionals.
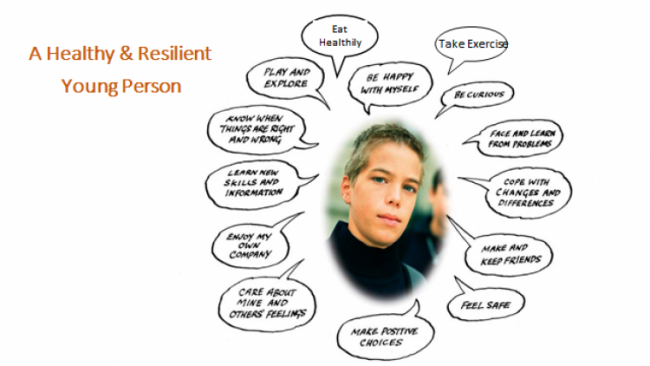
A Healthy Child
A Child or Young Person with Positive Mental Health and Wellbeing should show most of the following characteristics. Deficits in any particular area might compromise Wellbeing causing further Social, Emotional and Behavioural concerns to manifest.
Use this to help when undertaking assessments and to explore/identify areas of strengths and difficulties
Aid Memoire Check list
The following aid-memoir for gathering information can help with undertaking an assessment and knowing what to ask. This can also help identify a context to the concern and indicate what sort of intervention is required:
1. What is the concern about?
Safeguarding, Behaviour, Emotion, Educational, Social, Physical, Mental, Cognitive, Combination?
2. What is the concern about specifically i.e. how does it present, how does it affect daily life, what does it relate to and how serious is it*?
Presentation
Safeguarding, Behaviour, Habit, Fear, Self-Harm, Confidence, Low Mood, Misconduct, Panic, Post-Traumatic stress, Obsessions, Anxiety-(Separation ,Generalised, Social)
Impact
Development, Concentration, Learning, Restlessness, Functional Abilities, Performance, Thinking, Relationships
Contributing Reasons
Adjustment to Life Events, Loss, Domestic Violence, Safeguarding, learning Difficulty, ADHD, ASD, Dyspraxia, Dyslexia, Parent/Carer Ill Health
*Refer to the Thresholds and Pathways Document/Seek Consultation.
3. How long and frequent has the issue been a concern?
Safeguarding, Behavior, Emotion, Educational, Social, Physical, Mental, Cognitive, Combination?
4. Who else Knows or needs to know about the concern?
Parent/Carer/Family Member, Friend, Teacher, Professional
5. Is it safe, appropriate or a statutory requirement to liaise with or, include others in supporting the concern?
Teacher, Parent/Carer, Consultation with RMC or MASH etc
6. What has been tried to manage the concern?
Relaxing, Talking to Someone, Using Strategies/Distractions, Hobbies/Interests/Clubs/On-Line Information. Additional Support etc
7. How Successful was the use of Self-Management Techniques or Additional Support?
Could anything similar be tried again?
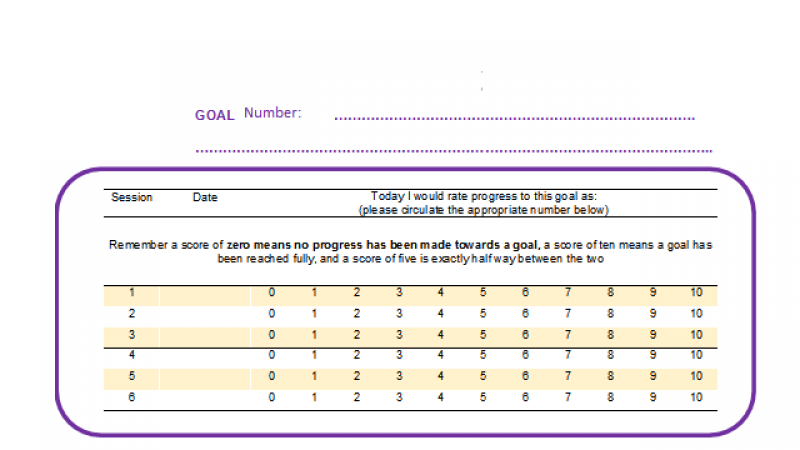
8. What needs to be achieved?
Goal Setting
Stop/Control Something i.e. behavior, habit, worry, self-harm.
Achieve Something i.e. confidence to do something, make friends, worry less, organise tasks
Self-Management
Protective behavior strategies, Talk to someone, learn relaxation and distraction techniques
9. What and Who could help support the concern and in what way?
Clients Tasks
To See Someone to Help for a few times, keep a Diary, Set Goals to achieve, use Self-Rating to chart progress made, Positive Thinking, learn a Social Skill, Observe Role-Models for managing or trying something new. Access School Drop-In service.
Helpers Tasks
Use of outcome measures, Help to think through ideas and what Tasks to try, Explore Options/Choices, Rehearsing/Role-playing what to do. Encourage and give Feedback. Facilitate other support systems – School staff/Family members, Individual Education Plan, Pastoral/Peer support, further Assessment-Health Education and Care Plan- Consultation with RMC or MASH etc
10. How will a positive outcome be measured and an individual is managing better within their capacity to do so?
Review
Goals achieved, happier, reflect how things have changed, considers how to manage in the future.
Evidence
concerns improved, less frequent or ceased, new things tried and met with success, correct support systems in place, Outcome measures rate improvement etc.
Evidenced Based Practice & What a Typical Individual Intervention Session should look like:
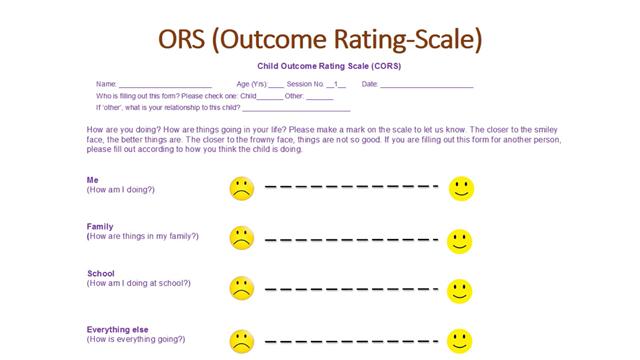
Adverse Childhood Experience Studies (America 95/97+Longitudinal) showed that the use of Outcome Rating-Scales, Goal Setting used in a Supporting (Alliance) Helping Relationship Allegiance) can promote individual’s recovery, with less time spent attending services.
Evidenced Based Practice is being recommended across all agencies and Service levels.
Outcome Measures and assessment tools contained within IAPT (Improved Access to Psychological Therapies) for Children and Young People is one major recommendation and is cited in most recent Agendas.
NICE Guidelines for Social and emotional wellbeing in primary education
Examples of Adverse Childhood Experiences: -
- Emotional Abuse
- Physical Abuse
- Sexual Abuse
- Physical Neglect
- Emotional Neglect
- Alcoholic in Household
- Drug User in Household
- Experiencing Domestic Violence
Factors accounting for success:
- Technique - (doing) - 8%
- Allegiance - (supporting) - 30%
- Alliance - (relationship) - 60%
Use of Routine Outcome Measures’s (ROM’s) - i.e. Outcome Rating Scales (ORS) and Goal Based Outcomes (GBO’s)
- Increases rate of recovery and change
- Decreases length of time for support
- Greet the individual: review Self-Rating Scale and Goals Achievements (Or: set New Goals and commence a Self-Rating Scale if this is the first session) See: goal setting and Outcome Rating Scale in the next section.
- Explore themes from Self-Rating Scale and Goals Achievements, use problem solving to explore strategies, use intervention tools, worksheets and information sheets. See >Psychologytools.org in the Support Section
- Set tasks to be tried, receive feedback for how this session went, set next date. Session feedback form. (Awaiting This)
The table below shows the protective factors that can make it more likely for a pupil to deal with adversity while maintaining good mental health.
The risk factors indicate the greater likelihood of a pupil finding it hard to maintain good mental health. The greater the number of risk factors and fewer protective factors, the more likely a pupil is to have a mental health difficulty.
The balance of risk and protective factors can affect pupils’ coping skills and their emotional well-being. However, this balance can be changed and resilience can be enhanced by providing appropriate resources and experiences.
These coping skills can be taught and learnt.
Research has shown that there are a number of risk factors that increase the chances of adolescents developing health and behaviour problems. Equally important is the evidence that certain protective factors can help shield youngsters from problems. If we can reduce risks and increase protection throughout the course of young people's development, we can prevent these problems and promote healthy, pro-social growth.
The following graph supports a public health model using a theoretical framework of risk reduction and protection enhancement. Developments in prevention and intervention science have shown that characteristics of individuals, their families, and their environment (i.e., community neighbourhoods, schools) affect the likelihood that individuals will engage in substance abuse, delinquency, violence, and school dropout. Other characteristics serve to protect or provide a buffer to moderate the influence of the negative characteristics. These characteristics are identified as risk factors and protective factors.
Promoting Resilience
It is Important to Help Build Resilience in Young People in order for them to:
- Promote and Maintain; Their Emotional Wellbeing and Mental Health
- Develop Self-Awareness
- Develop Self-Reliance
- Have Ownership of Thoughts
- Have a Perspective of Self and Others
- Develop the Ability to Action-Plan and Problem-Solve
- Learn and Apply; Positive Coping-Strategies
- Make Constructive-Decisions
- Learn and Master; Impulse-Control and Emotional-Regulation
Promoting Resilience Involves
- Helping with the use of Communication, Practical Resources, Tools and Techniques. (To Enable; Exploring, Problem Identification, Problem-Solving, Goal Setting & Action)
- Help to Acquire New Skills; Develop Existing Skills and the Apply these Skills in practice. (Show-Tell-Do)
- Providing Essential; Knowledge, Information, Learning Tools and Techniques to Explore and Utilise to be able to Think-Constructively and Act-Positively.
- Interest, Motivate and Engage Young People to Help Empower them to Build their Confidence and learn New Skills
- Encourage and Support Young People to Adapt during Times of Stress and Adversity
- Promote Resilience and Capacity to Cope.
Promoting Resilience helps to:
It is Important to Help Build Resilience in Young People in order for them to:
- Promote and Maintain; Their Emotional Wellbeing and Mental Health
- Develop Self-Awareness
- Develop Self-Reliance
- Have Ownership of Thoughts
- Have a Perspective of Self and Others
- Develop the Ability to Action-Plan and Problem-Solve
- Learn and Apply; Positive Coping-Strategies
- Make Constructive-Decisions
- Learn and Master; Impulse-Control and Emotional-Regulation
Generalized Anxiety Disorder 7-item (GAD-7) scale
Over the last 2 weeks, how often have you been bothered by the following problems?
- 1. Feeling nervous, anxious, or on edge
- 2. Not being able to stop or control worrying
- 3. Worrying too much about different things
- 4. Trouble relaxing
- 5. Being so restless that it's hard to sit still
- 6. Becoming easily annoyed or irritable
- 7. Feeling afraid as if something awful might happen
- To view the full document click here
This is a self screening questionnaire for depression and anxiety. The patient should be instructed not to take too long over their replies: their immediate reaction to each item will probably be more accurate than a long thought-out response. Although it was designed for hospital General Medical Outpatients, it has been extensively used in Primary Care.
Your login details have been used by another user or machine. Login details can only be used once at any one time so you have therefore automatically been logged out. Please contact your sites administrator if you believe this other user or machine has unauthorised access.

